Real-Time Care, Real-Time Decisions
Why We Need to Fix Prior Authorization Now?
The fluorescent lights hum overhead, casting a sterile glow on the scene unfolding in the hospital room. Sarah, a vibrant young woman in her early thirties, coughs weakly, her once lively eyes clouded with fear. Dr. Patel, her oncologist, stands beside her, a grim expression etched on his face. He holds the results of a new clinical trial, a faint ray of hope in Sarah's fight against a rare form of cancer. But this hope dims as Dr. Patel explains the next hurdle – securing prior authorization from Sarah's insurance company for a treatment not yet widely adopted.
This scene, with variations, plays out countless times across the American healthcare landscape. Prior authorization, a system designed to control healthcare costs while improving patient health, ensuring that the patient's condition, diagnosis and medical treatment are in line to address patient health, often becomes a bureaucratic hurdle, trapping patients and providers in its frustrating coils. While the intent behind prior authorization is sound, the reality is far from simple.
The Frustration Cycle
Imagine a world where a doctor's hands are tied, their expertise rendered secondary to a checklist. This is the reality for many providers facing prior authorization roadblocks. A recent study published in JAMA Internal Medicine reports that nearly 90% of physicians reported experiencing delays or denials in prior authorization requests. These delays translate into postponed treatments, increased patient anxiety, and a demoralized healthcare workforce.
But the burden of prior authorization doesn't just fall on providers. Patients, already grappling with illness, are thrust into a world of medical codes and bureaucratic jargon. To effectively use their benefits and minimize their financial responsibility, they must become adept at navigating the intricate rules of their health benefit plan.
This requires knowledge of the available benefits, which providers are in their network, and how to exercise their appeal rights. Understanding these elements is essential for patients to manage their coverage and protect themselves against excessive costs.
Fortifying this, A 2021 survey by the Kaiser Family Foundation revealed that 45% of adults with private insurance had experienced prior authorization delays, leading to postponements in care or difficulty affording treatment.
Furthermore, the ripple effects of a broken prior authorization system extend beyond the doctor's office and the patient's bedside. Hospitals, caught in the crossfire of denials and delays, face significant financial strain. A study by the American Hospital Association estimated that hospitals spend billions annually managing prior authorization requests. These costs, coupled with potential revenue losses from unapproved treatments, can force some healthcare institutions to close their doors.
Contrary to popular opinion, insurers aren't happy either. They're flooded with requests, making fast approvals a challenge. Imagine if everyone used the same system—approvals would fly through! Denials for certain requests seem harsh, but they're fighting to keep everyone's premiums affordable. Just like everyone else, they want patients treated quickly but within a system that doesn't break the bank.
The sad truth is, that despite everyone in this cycle doing their all to ensure better care, the current system remains frustratingly clogged, leaving patients stuck in the waiting room.
A Deep Dive into the Current State of Prior Authorization
The landscape of prior authorization (PA) is complex and varied, reflecting a patchwork of processes that, while intended to streamline healthcare delivery and control costs, often achieve the opposite.
Third-Party Administrators (TPAs) and Business Process Outsourcing (BPOs): TPAs and BPOs help reduce administrative burdens for health plans by handling Prior Authorization (PA) processes. However, their reliance on standardized protocols can lead to nuanced misunderstandings and inappropriate care denials, as they often lack the flexibility needed for individual cases. This can necessitate costly appeals. Additionally, service quality varies, potentially leading to delays and communication issues, as providers deal with representatives not involved in direct patient care.
Manual In-House Operations: Many providers still use manual systems for PA, prone to human errors like misplaced documents and data entry mistakes. These systems consume significant staff time, detract from patient care, and can lead to staff burnout. As patient volume increases, manual PA becomes unsustainable without significant staffing increases, challenging economic feasibility.
Partially Automated Systems: While some providers and insurers use partially automated systems for routine PA requests, these systems often fall short with complex cases, requiring manual oversight. Such systems can create bottlenecks, prioritizing simpler cases and neglecting more complex, urgent ones. Integration issues with broader healthcare IT systems further hinder their effectiveness, creating data silos and communication challenges.
Complex Cases Overlooked: Current PA systems struggle with complex cases that need tailored scrutiny, often failing to address the unique needs of treatments involving rare diseases or innovative procedures. The lack of a flexible approach risks overlooking critical care aspects, potentially resulting in poor treatment outcomes.
Despite the digital advances in other areas of healthcare, the reliance on manual processes remains significant, imposing a substantial administrative burden on healthcare providers and introducing inefficiencies that can delay patient care and increase overall healthcare costs. Although several key players in the industry aim to revolutionize the PA landscape, the current market solutions have shown limited success in addressing the depth and complexity of medical necessity reviews, often struggling to effectively handle more complex medical scenarios that require detailed clinical understanding and decision-making.
Attempts to improve timely and effective solutions to complex cases with custom practices and process systems have also shown limits, given the high reliance on provider network agreements and selection criteria that include the cost of care in review by vendors. This often restricts the scope of possible improvements, maintaining the status quo of administrative challenges.
Automating Medical Necessity & Road to Real-Time Adjudication
Amidst this frustrating cycle of delay and the maze of primitive inventions, the push towards real-time adjudication of prior authorization emerges not only as a necessity but as a catalyst for profound change. This leap forward, powered by the CMS-0057-F final rule, heralds a transformative shift in how healthcare decisions are made—swiftly, seamlessly, and with the patient's urgent needs at the forefront and promises a radical simplification of healthcare bureaucracy
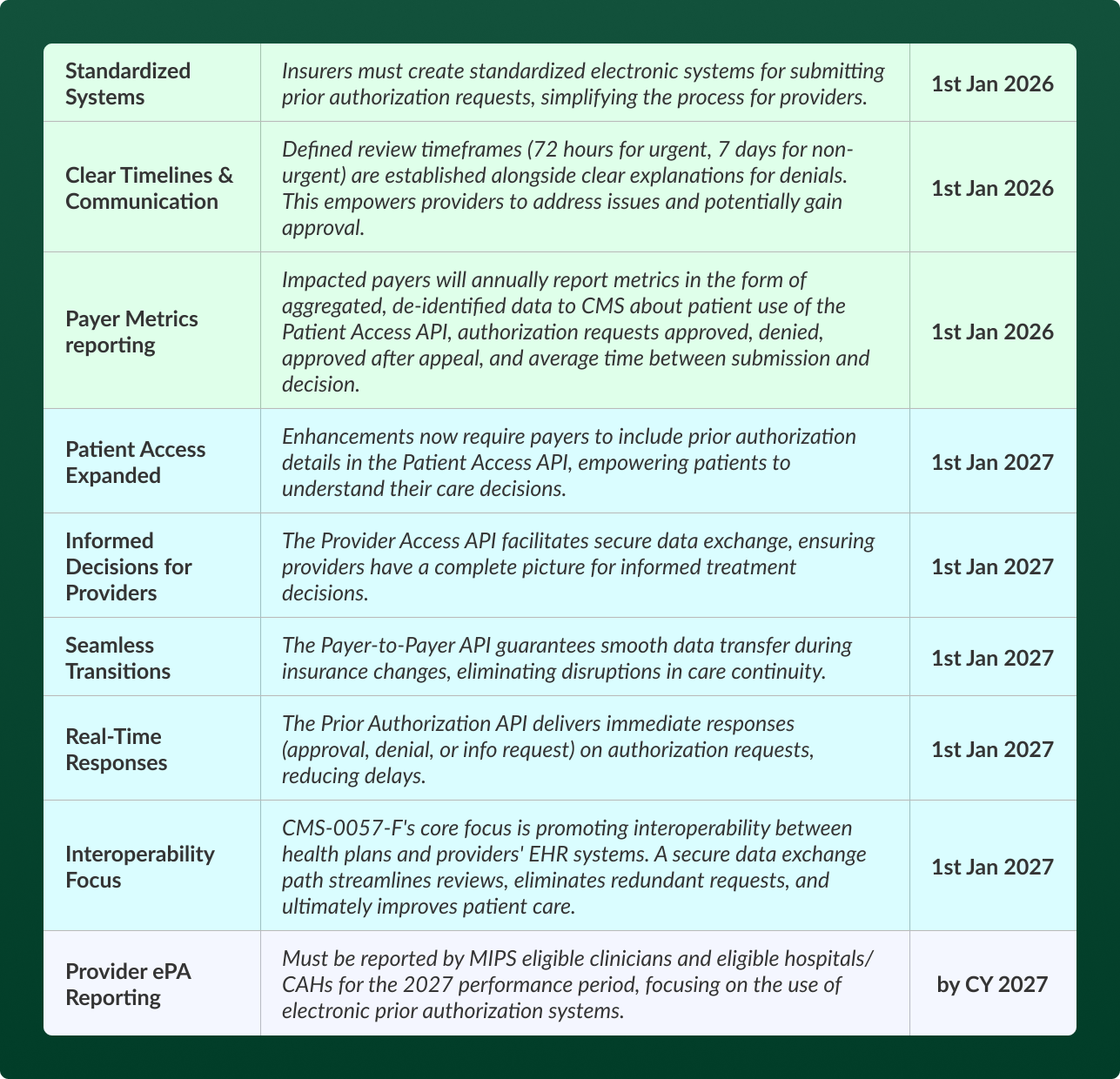
The CMS-0057-F final rule is instrumental in this vision. It mandates that Medicare Advantage, Medicaid, CHIP, and other federally facilitated exchange organizations adopt and maintain robust API systems to enhance the electronic exchange of healthcare data. This rule is not just about improving speed but also about ensuring interoperability and transparency across the healthcare spectrum.
Transitioning to real-time adjudication is not without its complexities. The technological overhaul required to support advanced APIs involves substantial financial investments. It demands a high level of technical acumen, presenting a significant challenge, particularly for smaller providers or insurers with limited resources. Additionally, increased data sharing necessitates stringent data security measures to protect patient privacy, complicating the implementation landscape and amplifying the need for smart-tech partners.
To fulfil the mandate and enhance healthcare outcomes, all stakeholders must collaborate closely, investing in and implementing system enhancements that swiftly remove existing impediments and barriers. This unified effort is essential for successfully transitioning to real-time adjudication, redefining healthcare efficiency and patient care.
A Smart Leap Forward with RISA
Today, when the need for efficient, real-time adjudication (RTA) is more pressing than ever, RISA emerges as a preeminent solution in this landscape, with its state-of-the-art Multi-Agent System. It elegantly marries the capabilities of large language models (LLMs) and Generative Artificial Intelligence (Gen AI) to offer a seamless, smart-tech partnership for health systems and health plans.
At the core of RISA's effectiveness are the AI Agents, powered by advanced LLMs, which excel in processing and interpreting complex human language. These agents are meticulously trained on extensive datasets that include medical literature, insurance policies, and historical prior authorization (PA) requests. Such training enables them to navigate the intricate details of medical terminology, clinical scenarios, and regulatory compliance with an exceptional level of precision. Consequently, RISA can adjudicate PA requests swiftly and with remarkable accuracy.
RISA’s AI agents for prior authorization are trained using historical claims data, prior authorization records, and patient medical histories, along with comprehensive analysis of insurance guidelines. Additionally, our in-house prior authorization associates provide valuable expertise and real-life healthcare insights for reinforcement learning.
RISA's use of Generative Artificial Intelligence (Gen AI) further enhances its capability. Gen AI transcends traditional, task-specific applications, offering broad-spectrum intelligence that simulates human analytical capabilities. By integrating with various healthcare IT systems, Gen AI facilitates a comprehensive and real-time consideration of all relevant patient data, from clinical histories to diagnostic reports. This integration ensures that RISA operates with minimal delays and errors, enhancing the overall efficiency of the PA process.
Driving Higher ROI with RISA
Incorporating these advanced technologies, RISA not only streamlines operations but also significantly enhances the potential for a higher return on investment (ROI) in healthcare. By automating the prior authorization (PA) process, RISA dramatically cuts administrative overhead, freeing up resources for critical, high-value tasks. RISA’s precise medical necessity assessments minimize the occurrence of costly denials and appeals, smoothing financial operations and easing the burden on healthcare systems.
To capitalize on these efficiencies further, the RISA solution includes automated results measurement and performance monitoring through online, real-time compliant dashboards. These dashboards are accessible to all stakeholders and provide continuous updates during startup and throughout warranty periods. By sharing data analytics that highlights trends, patterns, and gaps, RISA enables stakeholders transparency and ensures smoother operations but also plays a vital role in improving patient outcomes and satisfaction, thereby enhancing patient retention and the overall reputation of healthcare providers.
Healthcare’s future - Enhanced, Unified System Efficiency
The time is now! The CMS-0057-F final rule sets a bold agenda for change.Providers and payers are responsible for ensuring clear communication, advocating for standardized forms and user-friendly technology that integrates seamlessly with real-time authorization platforms.
In the payer space, provider network management operations are critical in continuously educating providers and addressing rework and abrasion situations. It is also crucial to educate patients about their plan policies and appeals processes, emphasizing the importance of minimizing time lost in administrative procedures.
Payers should invest in technology for robust API integration and real-time data exchange, developing clear, evidence-based criteria for approvals and denials while maintaining transparency with providers and patients.
Patients are key players in managing their health care, and it's crucial that they proactively understand their plan's prior authorization policies and work with their doctors to navigate the process. To support this, payers must create effective communication streams and share authorization information in a simplified and transparent manner, such as through enhanced user portals and telephony mechanisms. This enables patients to advocate for themselves when necessary, utilizing online resources and patient advocacy groups to ensure they receive the care they need.
The Need for Unified Action
This isn't just about streamlining—it's about transforming healthcare delivery.
In this transformative process, pivotal contributions come from partners like RISA, whose advanced AI-driven technology and partnership provides the necessary backbone for future readiness, playing a key role in driving forward this unified vision.
Imagine a future where patients like Sarah receive timely treatment without bureaucratic delays, where doctors like Dr. Patel are empowered by real-time approvals to focus on providing care, and where the healthcare system values efficiency and empathy equally. Achieving this future demands a collective effort to break down silos, foster collaboration, and leverage the right technology to construct a healthcare system that benefits everyone.
References
AMA Digital Health Care 2022 study findings. American Medical Association. (2022, September 28).
Fact sheets CMS interoperability and Prior Authorization Final Rule CMS-0057-F. CMS.gov Centers for Medicare & Medicaid Services. (n.d.).
Fumiko Chino, M. (2023, October 18). Patient experience of prior authorization for cancer care. JAMA Network Open.
Karen Pollitz, K. P. (2023, October 12). Consumer problems with prior authorization: Evidence from KFF survey. KFF.
Patients and physicians speak out. Prior Authorization. (n.d.).
Regulatory overload report: AHA. American Hospital Association. (n.d.).
Tong, N. (2024, February 22). Ma enrollees constrained by Prior Auth but docs more likely to ask about health assessments: Report. Fierce Healthcare.